A model for cellular disease transitions: As detailed below, our model for disease state transitions proposes that certain cellular stress responses become overwhelmed under chronic stress conditions, leading to dysregulation of the major quality control (QC) hubs required to maintain cell fate homeostasis. Specifically, we hypothesize that the major disease specific QC hubs lie at the intersection between nuclear and the endoplasmic reticulum (ER) homeostasis. The first major prediction is that “stressors” associated with disease states will preferentially affect nuclear functions (i.e, genome stability, transcriptional networks, ribosome biogenesis and nuclear import/export pathways) and primary lipid metabolism centered on the ER but connected to other major membrane organelles (i.e., lipid droplets, mitochondria, the nucleus and xxx). The second major prediction is that disease transitions will result in the alteration of cell stress response pathways designed to maintain nuclear and ER homeostasis (i.e., autophagy, proteostasis). The final major prediction is that chronic stress is defined by a combination of individual stressors or the accumulation of periodic, sustained stressors.
Cellular disease states: Many of our research questions surrounding genome integrity and chromosome instability in cancer led us to rethink the way we frame the questions we have been investigating. What are the steps involved in a normal cell transitioning to a disease state? Though this very broad question is difficult to answer with a single experimental approach, it has led us to formulate a model that is testable using simple to more complex cellular model systems. Many investigators of disease have turned their attention to cell stress pathways and the downstream inflammatory response that lead to more physiological inflammation associated with disease. At the physiological level, investigators like Bruce McEwan have described the physiological response to stress in the context of an “allostatic load” — the idea is that the same physiological stress response that can protect us in the short-term can lead to long-term damage that is associated with chronic disease. The fascinating implication of the concept if allostasis is that it uses a response model that is identical to the cell signaling models we are all familiar with (see figure below from the linked McEwan article NEJM). The idea that a physiological stress causes an “activation” step, followed by “amplification” and “recovery” mirrors that way that cells respond to cues, including cellular stress.

At a physiological level, chronic disease arises from repeated stress “hits” and a prolonged stress response or a failure of the physiological response to “adapt” and a resulting inadequate response. We borrowed the idea of allostatic load to apply to the cellular states that must precede the physiological response. In our model, cells respond to changes in homeostasis (i.e., stress) by activating various pathways, amplifying the signal and then down regulating the response to return to homeostasis. Frequent cell stress or prolonged stress can lead to aberrant stress responses which initiate alterations in cell programming, activation of inflammatory signals (at least in metazoans) and progression to a disease state. In my lab, we are using this model to understand how specific cellular stress associated with DNA replication and protein misfolding activate cell stress pathways and lead to reprogramming of the ability of cells to respond and thus the progression to disease states. We are probing these ideas in the context of cancer progression that might arise from DNA replication stress but also from the context of neurodegenerative disease associated with proteotoxic stress. We are particularly interested in the intersection between these two different forms of cell stress and how each might contribute to cellular disease states.
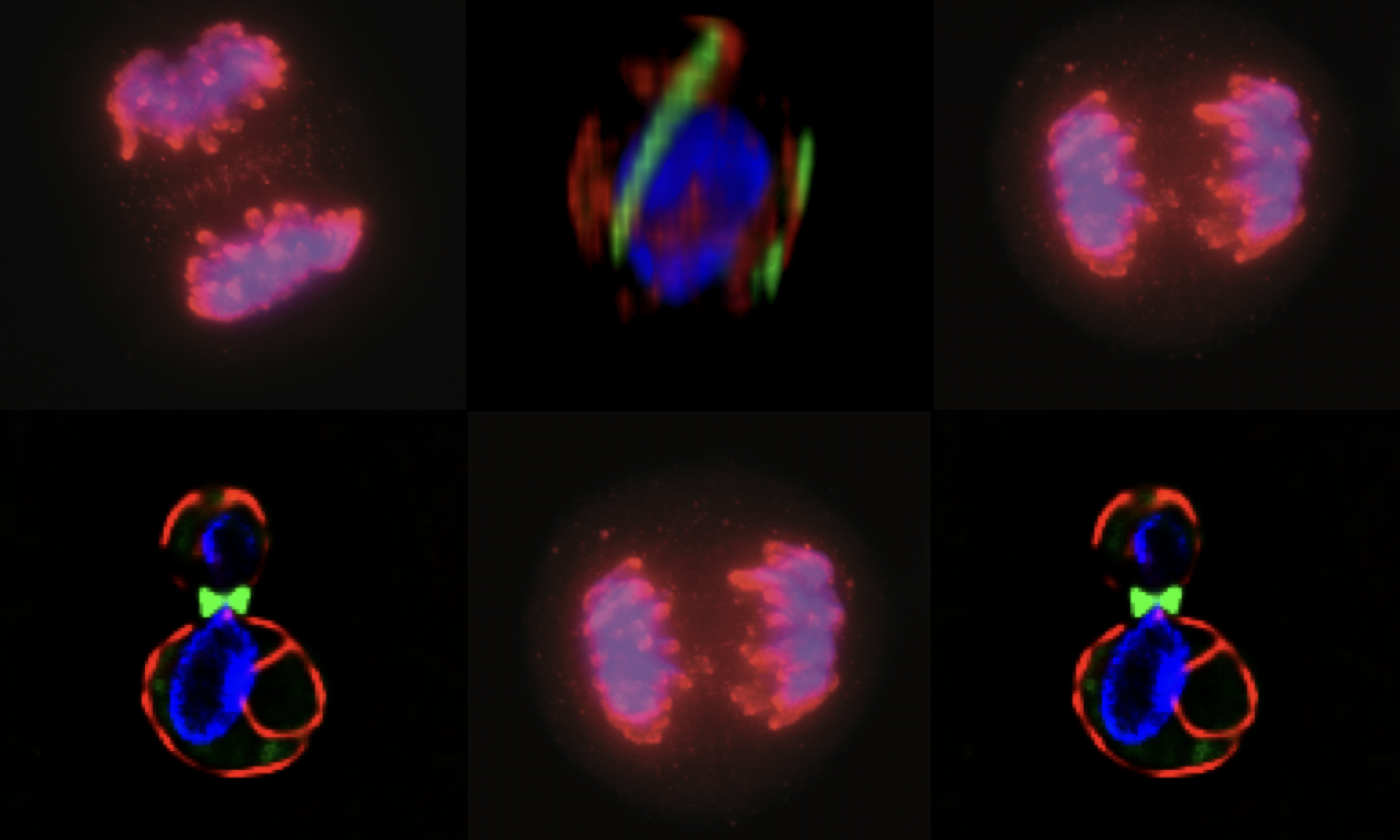
A cellular disease model system: There are arguably many ways to interrogate how cells respond to chronic stressors, but we have chosen to model this in the unicellular eukaryote, S. Cerevisiae, or budding yeast. Though lacking some of the complexity of mammalian cells, it shares a remarkable degree of conservation at the level of nuclear and ER homeostasis. There are currently two major approaches in the lab to model disease related stress: (i) we are using genetic and pharmacological approaches to transiently delay DNA replication to mimic the kind of stress cancer cells experience with too many chromosomes, and (ii) we are modeling neurodegenerative disease associated stress by conditionally expressing human alpha-synuclein that we and others have shown induces ER stress. Both of these disease-associated stressors converge on the set of QC-autophagy pathways that are important for maintaining nuclear and ER homeostasis.
How do these pathways respond to transient vs chronic stressors and how do changes in these pathways support disease progression?